Your cart is empty
The Ultimate Guide to Gastric Banding Surgery
What is Gastric Banding Surgery
Gastric banding surgery is a weight loss procedure that uses an adjustable band placed around the upper part of the stomach to restrict food intake, promoting significant weight loss. It's one of the least invasive bariatric surgery options available today.
For those struggling with severe obesity and unable to lose weight through diet and exercise alone, gastric banding can be an effective, low-risk approach. This guide will walk through everything you need to know about gastric banding, how it works, expected results, lifestyle impacts, and more.
Who is a Candidate for Gastric Banding?

Gastric banding may be an option for adults with:
- A BMI of 40 or more (severe obesity)
- A BMI of 35 or more plus an obesity-related health condition like diabetes or high blood pressure
- The ability to fully commit to required lifestyle changes
Gastric banding is not recommended for patients who have certain health issues that may interfere with surgery or recovery. Your bariatric surgeon will conduct a complete assessment to determine if you are a good candidate.
How Does Gastric Banding Promote Weight Loss?
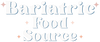
Gastric banding gets its name from the adjustable band that is placed around the upper part of the stomach during surgery, essentially separating the stomach into a small upper pouch and a larger lower part. It restricts how much food can pass from the pouch into the rest of the stomach, promoting early satiety with smaller meal portions.

Gastric band creates a small stomach pouch
The band is connected to an access port that is placed under the skin during surgery. The gastric band can be tightened or loosened over time by adding or removing saline via the access port. This adjustability is a key benefit of gastric banding.
What Are the Benefits of Undergoing Gastric Banding Surgery?
There are many potential benefits associated with gastric banding for weight loss:
-
Significant long-term weight loss: Patients can expect to lose 50-60% of their excess body weight over 2 years. This compares favorably to the typical 60-80% excess weight loss from more invasive procedures like gastric bypass surgery and gastric sleeve surgery.
-
Less invasive procedure: Gastric banding does not require any stomach cutting or stapling. This leads to fewer risks during surgery, a faster recovery, and lower chance of long-term vitamin deficiencies.
-
Adjustability: The band can be tightened or loosened as needed to fit your new lifestyle and help you continue losing weight. This level of customization is unique to gastric banding procedures.
-
Reversibility: Although uncommon, the gastric band can be removed entirely through a minimally invasive procedure. This cannot be done with bypass or sleeve gastrectomy.
-
Low mortality risk: Gastric banding mortality risk is less than 0.1%, much lower than the 0.5% risk from more complex bariatric surgery procedures.
What Are the Risks and Drawbacks of Gastric Banding?
While considered low-risk, gastric banding does come with some potential drawbacks to consider:
-
There is a risk of the band eroding or slipping out of position, which would require revisional surgery. This occurs in about 5% of gastric banding patients.
-
Weight loss from gastric banding may plateau sooner and result in less total weight loss compared to other procedures over the long term.
-
Dietary restrictions must be followed life-long to prevent band-related complications. Grazing and eating unhealthy foods can be dangerous.
-
Frequent follow-up visits and potential band fill adjustments are required to ensure optimal results. This demands a strong commitment to aftercare.
How Should I Prepare for Gastric Banding Surgery?
Thorough physical and mental preparation is vital to ensure the best results from your gastric banding procedure. Here are some top tips:
Follow the pre-op diet: Most bariatric programs require following a liver shrinking or very low-calorie diet for up to 6 weeks before surgery. This helps reduce liver volume to ensure the best surgical access.
Quit smoking: Smoking severely increases surgical risk and impairs healing. You must quit smoking for at least 6 weeks prior to your procedure.
Get key health issues under control: Conditions like diabetes, heart disease and lung disease can increase surgical risks. Work closely with your doctors to optimize all health issues before your operation.
Secure insurance clearance: Most insurers cover gastric banding given clear medical necessity for bariatric surgery. Double check that all approvals are in place prior to scheduling your procedure.
Find the right bariatric surgery team: A skilled, experienced bariatric surgeon and comprehensive aftercare program give you the best chances of meeting your post-op health and weight loss goals. Do your research.

What Does the Gastric Banding Procedure Involve?
Gastric banding surgery is performed laparoscopically, meaning it uses minimally invasive techniques rather than open abdominal surgery. Here is how the typical procedure goes:
-
General anesthesia is administered to keep the patient fully unconscious during surgery.
-
The surgeon inserts narrow, lighted tubes with cameras through 5 small (1 cm) abdominal incisions. Surgical instruments are also placed through these access ports.
-
The upper part of the stomach is wrapped with the deflated gastric band. The band circumference can be adjusted with an internally threaded mechanism.
-
The access port is connected to the gastric band tubing and placed under abdominal skin for band adjustments after surgery.
-
After checking for proper positioning and band security, the surgeon closes all incisions with absorbable sutures or surgical glue.
The laparoscopic gastric banding procedure typically takes 1-2 hours to complete. Patients usually stay 1 night in the hospital before being discharged if there are no complications. Most patients can return to normal daily activities within 1 week.
What is Recovery Like After Gastric Band Surgery?
During initial gastric banding recovery:
- A liquid diet is slowly progressed for 2-4 weeks post-surgery.
- Prescribed pain medications help keep patients comfortable.
- Follow all instructions for wound care, walking, breathing exercises and band adjustments.
- Avoid rigorous activity for 4-6 weeks until healing is complete.
After recovering from surgery, the real work begins with adopting all required diet, exercise and lifestyle changes.
Adapting to Your New Diet & Lifestyle
Life with a gastric band requires dedication to a new, long-term approach to eating:
-
Follow your diet progression plan: Slowly advance from clear liquids to soft foods as directed by your dietitian to prevent malnutrition. Lifelong vitamin supplementation is vital.
-
Develop healthy eating habits: Your new stomach pouch limits food intake. Small, frequent, high-protein meals are key. Chew thoroughly and stop eating at the first feeling of fullness to avoid discomfort.
-
Avoid problematic foods: Steer clear of fibrous, sugary or tough-to-digest foods that can obstruct your gastric band. Follow all nutritional guidelines from your bariatric physician or dietitian.
-
Exercise for fitness and weight loss: While exercise cannot compensate for poor diet, building cardio, strength and flexibility helps boost metabolism and tone body composition. Aim for at least 30 minutes of activity daily.
-
Seek emotional and social support: Support groups, whether online or in-person, provide the camaraderie and understanding needed to help you through challenges adjusting to life after bariatric surgery.
What are the Long-Term Outcomes of Gastric Banding?
Patients who closely adhere to gastric banding post-op guidelines typically continue to lose weight steadily in the first 1-2 years after surgery, achieving 50-60% excess body weight loss. Many patients report remission of type 2 diabetes, high blood pressure and other obesity-related diseases as well.
Some gastric band patients may require one or more band adjustments during follow-up appointments to tighten or loosen the band and promote further weight loss. Although less common with gastric banding than more invasive surgeries, some patients develop sagging excess skin that interferes with daily activities. Plastic surgery, such as a body lift, can remove and tighten excess skin.
Over the long term (10+ years), a subset of gastric band patients experience diminished weight loss results or band-related complications necessitating band removal. However, the vast majority successfully manage their bands and maintain significant weight reductions. Smaller European studies show 40-50% of excess weight loss persisting beyond a decade post-op.
Is Gastric Banding Right For You?
We've covered all the key details about gastric banding surgery. The ultimate question is whether gastric banding is the best weight loss option in your personal situation. Gastric banding offers exceptional results for the right patients – those fully prepared for the commitment required. We encourage you to speak with a bariatric surgeon to decide if a gastric band could be your key to lasting weight loss success.
Read Next: The Best Bariatric Protein Shakes
Author: Allison Allison, a certified nutritionist and research author, brings over 15 years of experience in the health and weight loss industry. Allison's influence extends through her authorship of multiple health and wellness journals, where she shares her expertise and research on medical weight loss and bariatric medicine. |
Reviewed & Edited By: Dr. K. Huffman Dr. Kevin D. Huffman, D.O., is a board-certified bariatric physician renowned for his expertise in treating obesity. With over 10,000 patients and a reputation as a national leader in bariatric medicine, he has trained hundreds of healthcare providers. As the founder of American Bariatric Consultants, Dr. Huffman develops protocols and training materials sought after by medical societies, pharmaceutical companies, patients, and hospitals. |
Bariatric Guides & Information
More Info
Customer Favorites
- Choosing a selection results in a full page refresh.